Wellington
Subarachnoid Diverticulum
Home » Case Studies » Wellington
This is Wellington, a 12-year-old neutered male Pug with a 2-month history of ataxia (wobbliness) in the pelvic (rear) limbs. Signs came on slowly and worsened over two months.
Wellington's Initial Examination
Note how he is weak and wobbly in the pelvic limbs. His movements are robotic, and he is crouched in his pelvic limbs. Based on the normal mentation, cranial nerves and thoracic limbs, the weak pelvic limbs, normal spinal reflexes but absent postural reactions, we can say that he has a neurological problem affecting his T3-L3 (mid-back) spinal cord that is of moderate severity.
Based on his signalment (older male Pug), history (chronic, progressive, non-painful) and neuroanatomical localization, we can formulate a reasonably short list of possible causes.
Intervertebral Disc Disease (IVDD), cancer, meningomyelitis, malformation, degenerative myelopathy, syringomyelia, and subarachnoid diverticulum are all reasonable differentials.
Magnetic resonance imaging (MRI) of Wellington’s thoracolumbar spine was performed.
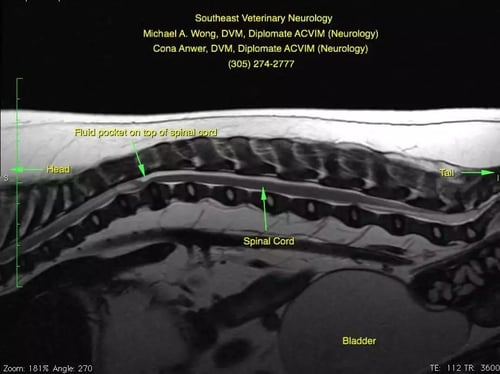
Wellington's MRI
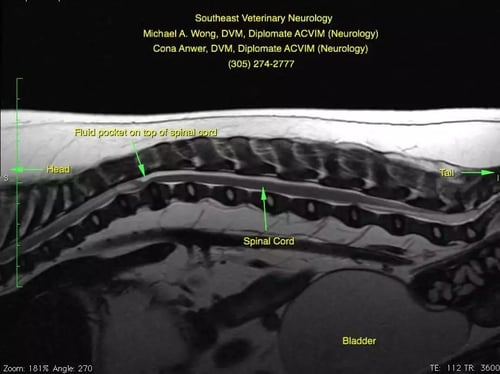
Wellington has a fluid buildup dorsal to the spinal cord that is compressing the spinal cord ventrally. Additionally, cranial to the dorsal buildup of cerebrospinal fluid (CSF), you can see that there is increased signal (“brightness”) within the spinal cord. This is the ‘classic’ finding of a relatively newly recognized disease. There are several different names that neurologists have used for this disease including “Pug Myelopathy”, “Pug Constrictive Myelopathy”, “facet hypoplasia”, “subarachnoid diverticulum” and others. Although little is published about this condition, in my experience, it is the most common cause of mid-back spinal cord problems in Pugs.

Wellington's Surgery

Since so little is known about the condition, there is no consensus among neurologists about the best way to treat it. My (Dr. Wong) experience has been that early surgical intervention carries the best chances of helping. Surgery is challenging, in that it involves a hemi- or dorsal laminectomy, durotomy/durectomy, gentle breakdown of the constriction and stabilization of the spine.
Dr. Wong is using an operating microscope which aids in lighting and magnification which is essential when performing this particular surgery (e.g. durotomy/durectomy and removing the ‘scar tissue’ from the subarachnoid space. The operating microscope is located in the upper left of the screen. The viewing screen in the upper right of the photo is similar (lower resolution) to what Dr. Wong sees through the microscope. In the viewer, cranial is to the left of the viewing screen and caudal is to the right. You are looking at the vertebral column. Two screws have been placed caudally and a third screw is being placed. Wellington is at the bottom of the screen, where you can see Dr. Wong’s hands and the drill.
Post-operatively, radiographs are performed to confirm accurate placement of the implants.
Many dogs with subarachnoid diverticula (Pug constrictive myelopathy/facet hypoplasia) do very well with surgery. Relapses are possible, but in my experience, they typically happen 2-3 years later. Unfortunately, not enough is known to make strong recommendations.
Post Surgery
We are happy to report that we re-examined Wellington this past week (seven months post-operatively) and he remains normal.
There are several important “Take Home” points that Wellington has illustrated for us:
- The most common cause of pelvic limb weakness in older Pugs is a poorly-characterized condition called “Subarachnoid Diverticulum,” “Pug Constrictive Myelopathy,” “Pug Ataxia,” or “Pug Facet Hypoplasia.”
- Fecal incontinence may sometimes be seen with mid-back (T3-L3) spinal cord problems and does not always indicate a lower (L4-S3) spinal cord problem.
- MRI is the gold-standard for viewing the spinal cord and nervous system. X-rays, myelography and computed tomography (CT) scans will not completely/accurately diagnose this and many other neurological conditions.